

28. July 2017
diagnosing and treating lower back pain with help of physio professionals
Diagnosing and treating lower back pain with the help of physiotherapy professionals offers a comprehensive approach to one of society's most common health complaints. Nearly 80% of adults experience lower back pain at some point in their lives, ranging from mild discomfort to debilitating conditions that significantly impact daily activities and quality of life. What many don't realize is that finding effective relief requires more than just addressing symptoms—it demands a thorough understanding of the underlying causes specific to each individual.
At CK Physiotherapy, we believe that proper diagnosis forms the foundation of successful treatment. Our chartered physiotherapists combine clinical expertise with advanced diagnostic techniques to identify the precise source of your pain, whether it stems from muscular tension, joint dysfunction, or more complex conditions. This evidence-based approach allows us to develop personalized treatment plans that not only alleviate current discomfort but also prevent future recurrence and promote long-term spinal health.
Understanding Lower Back Pain: Causes and Types
Different Types of Lower Back Pain (Acute vs. Chronic)
Lower back pain typically falls into two main categories: acute and chronic. Acute pain develops suddenly, often following a specific incident like lifting a heavy object or a sports injury, and generally resolves within 4-6 weeks with appropriate care. This type of pain serves as your body's warning system, signaling tissue damage that needs attention.1 Chronic pain, by contrast, persists for 12 weeks or longer, even after the initial injury has healed. This persistent discomfort may indicate ongoing inflammation, nerve sensitization, or structural changes that require more comprehensive treatment approaches.
Common Causes (Lifestyle Factors, Injuries, Medical Conditions)
Many factors contribute to lower back pain, with lifestyle elements often playing a significant role. Sedentary behavior, poor posture during prolonged sitting, and inadequate core strength can place excessive stress on spinal structures. Occupations requiring repetitive movements, heavy lifting, or prolonged standing similarly increase risk. Specific injuries like muscle strains, ligament sprains, and disc herniations frequently trigger acute episodes, while medical conditions such as degenerative disc disease, facet joint arthritis, and spinal stenosis typically produce more persistent symptoms.2 Other contributing factors include obesity, which increases mechanical load on the spine, and stress, which can heighten pain perception through muscle tension and nervous system sensitivity.
Warning Signs That Require Immediate Attention
While most lower back pain responds well to conservative management, certain symptoms warrant urgent medical evaluation. These "red flags" include severe pain that worsens when lying down, pain accompanied by fever, unexplained weight loss, or recent trauma like a fall. Particularly concerning are symptoms suggesting nerve compression: numbness or tingling extending down one or both legs, progressive muscle weakness, or changes in bladder and bowel function.3 These signs may indicate serious conditions such as cauda equina syndrome, spinal infection, or fracture that require immediate intervention beyond standard physiotherapy care.
Misconceptions About Lower Back Pain
Many misconceptions about lower back pain lead to unnecessary fear and inappropriate management. One common myth is that pain always indicates serious damage—in reality, pain intensity often doesn't correlate with tissue injury severity. Another misconception is that bed rest promotes healing; current evidence strongly supports maintaining reasonable activity levels. Many patients believe imaging like MRIs should be routine for all back pain, yet studies show that unnecessary scans can lead to overtreatment without improving outcomes.4 Perhaps most importantly, the belief that back pain inevitably becomes chronic is unfounded—with proper assessment and targeted treatment, most individuals achieve significant improvement and return to normal activities.
Professional Diagnosis: How Physiotherapists Identify the Source of Pain
Initial Assessment and Patient History
The diagnostic journey begins with a comprehensive initial assessment, where a skilled physiotherapist gathers critical information about your pain experience. This conversation explores the pain's onset (sudden or gradual), duration, quality (sharp, dull, burning), and pattern (constant or intermittent). Important contextual details include aggravating and relieving factors, previous treatments attempted, and how symptoms affect daily activities.1 Your physiotherapist will also inquire about your general health history, including previous injuries, surgeries, and existing medical conditions that might influence your current symptoms. This detailed patient history helps establish the foundation for a targeted physical examination and provides valuable clues about potential pain sources that might otherwise be missed.
Physical Examination Techniques
Following the history, your physiotherapist will conduct a thorough physical examination using specialized assessment techniques. This typically includes observing your posture and movement patterns, evaluating range of motion in the lumbar spine and related regions, and testing muscle strength and flexibility. Palpation (manual examination) of specific structures helps identify areas of tenderness, muscle spasm, or joint dysfunction. Neurological testing assesses nerve function through reflexes, sensation, and muscle response. Special tests like the straight leg raise or slump test can identify nerve root compression, while provocative maneuvers may temporarily reproduce your symptoms to help pinpoint their source.2 This systematic approach allows physiotherapists to develop a comprehensive understanding of your condition beyond what any single test could reveal.
When Imaging Is Necessary (and When It Isn't)
Contrary to common belief, advanced imaging isn't routinely needed for most lower back pain cases. Current clinical guidelines recommend imaging only when specific criteria are met: symptoms lasting beyond 6 weeks despite appropriate treatment, presence of neurological deficits, suspected serious pathology (infection, fracture, or malignancy), or when considering interventional procedures.3 This selective approach acknowledges that many imaging findings (like disc bulges or mild arthritis) appear in pain-free individuals and may not explain symptoms. Unnecessary imaging can lead to anxiety, overtreatment, and increased healthcare costs without improving outcomes. Your physiotherapist will determine whether imaging would provide valuable diagnostic information based on your specific presentation rather than as a routine first step.
Differential Diagnosis Approaches
Skilled physiotherapists employ differential diagnosis—a systematic process of distinguishing between conditions with similar symptoms—to accurately identify your pain source. This approach considers whether symptoms originate from musculoskeletal structures (muscles, joints, discs), neurological involvement (nerve roots, spinal cord), or potentially serious conditions requiring medical referral. Pattern recognition plays a key role, as certain symptom clusters often suggest specific diagnoses. For example, pain worsening with forward bending might indicate disc involvement, while pain during extension could suggest facet joint issues.4 Physiotherapists also evaluate whether symptoms might stem from regions outside the lower back, such as the hip or sacroiliac joint, which can refer pain to similar areas. This comprehensive diagnostic approach ensures that treatment addresses the true source of pain rather than just the symptoms.
Evidence-Based Treatment Options for Lower Back Pain
Manual Therapy Techniques
Manual therapy encompasses a range of hands-on techniques that physiotherapists use to improve tissue mobility, reduce pain, and restore normal function. Joint mobilization and manipulation involve carefully applied forces to spinal segments to improve movement quality and reduce stiffness. Soft tissue techniques such as myofascial release, trigger point therapy, and therapeutic massage help address muscle tension and fascial restrictions that contribute to pain.1 Additionally, neural mobilization techniques gently move nerve tissues to improve their mobility and reduce sensitivity. Research consistently shows that these manual approaches, when applied by skilled practitioners and integrated within a comprehensive treatment plan, can significantly reduce pain intensity and improve functional outcomes. At CK Physiotherapy, our therapists select specific techniques based on your unique presentation, combining different approaches to maximize effectiveness.
Exercise Therapy and Rehabilitation Programs
Exercise therapy forms the cornerstone of effective lower back pain management, with strong evidence supporting its benefits for both acute and chronic conditions. Initially, gentle movement helps reduce pain and stiffness while encouraging normal tissue healing. As symptoms improve, specific exercises target core stability, spinal control, and movement patterns. Progressive strengthening of the back, abdominal, and hip muscles provides better support for spinal structures during daily activities.2 Flexibility exercises address muscle imbalances that may contribute to pain. Rather than prescribing generic "back exercises," your physiotherapist will develop a personalized program that considers your specific diagnosis, physical capabilities, and functional goals. This tailored approach ensures that exercises address your unique needs while gradually progressing toward more challenging movements as your condition improves.
Advanced Treatments (Including Shockwave Therapy and Electrotherapy)
For cases that respond inadequately to conventional approaches, advanced treatment options may provide additional benefits. Shockwave therapy applies acoustic pressure waves to tissues, stimulating increased blood flow, accelerating healing, and reducing pain in conditions like chronic tendinopathies and myofascial trigger points.3 Electrotherapy includes transcutaneous electrical nerve stimulation (TENS), which modulates pain signals, and therapeutic ultrasound, which delivers deep heat to tissues to improve circulation and extensibility. These technologies complement rather than replace core treatments like manual therapy and exercise. At CK Physiotherapy, we've invested in these advanced modalities to provide comprehensive options for patients with persistent or complex lower back conditions, particularly when conventional approaches alone have yielded insufficient improvement.
Self-Management Strategies for Pain Relief
Empowering patients with effective self-management strategies is essential for long-term success. Heat therapy, using warm towels or heating pads, can relax tense muscles and increase tissue extensibility, while cold therapy helps reduce inflammation during acute flare-ups. Proper body mechanics during daily activities—from sitting posture to lifting technique—prevents unnecessary strain on recovering tissues.4 Pain-relieving positions, such as lying with knees supported or gentle stretches, provide immediate relief during painful episodes. Your physiotherapist will teach you how to recognize early warning signs of potential flare-ups and implement appropriate strategies before pain escalates. These self-management approaches complement in-clinic treatment, extending its benefits between sessions and providing you with greater control over your condition throughout your recovery journey.
Prevention and Long-Term Management: Beyond Pain Relief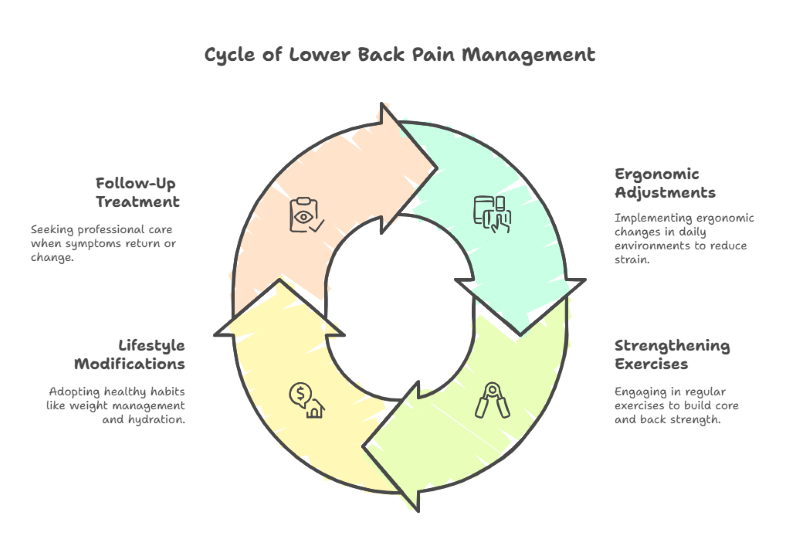
Ergonomic Considerations for Daily Activities
Addressing ergonomic factors in your daily environment plays a crucial role in preventing recurrent lower back pain. Workplace modifications such as adjustable chairs that support the natural spine curve, properly positioned monitors at eye level, and ergonomic keyboards can significantly reduce spinal strain during prolonged sitting.1 For those whose occupations require standing, anti-fatigue mats and appropriate footwear help distribute weight evenly and reduce pressure on the lower back. Home activities also benefit from ergonomic attention—adjusting kitchen counter heights, using long-handled tools for gardening, and selecting supportive mattresses that maintain proper spinal alignment during sleep. Rather than viewing these as temporary accommodations during recovery, consider them investments in long-term spinal health that can prevent future episodes and maintain the gains achieved through treatment.
Strengthening Exercises for Back Health
Maintaining a consistent exercise routine focused on key muscle groups provides the foundation for long-term back health. Core stability exercises that target the deep abdominal muscles, particularly the transversus abdominis and multifidus, create a natural supportive "corset" around the spine.2 Gluteal strengthening addresses a common weakness pattern that forces the lower back to compensate during daily activities. Functional exercises that combine movement patterns used in daily life—such as squatting, lunging, and rotating—train these muscles to work together efficiently. For optimal results, these exercises should progress gradually in difficulty and incorporate varied movements rather than focusing solely on isolated muscle groups. Evidence shows that individuals who maintain regular strengthening programs experience fewer recurrences and less severe episodes when compared to those who discontinue exercise after pain resolution.
Lifestyle Modifications That Support Recovery
Beyond specific exercises and ergonomic adjustments, broader lifestyle factors significantly influence lower back health. Maintaining a healthy weight reduces mechanical stress on spinal structures—even modest weight loss can substantially decrease symptoms in overweight individuals.3 Adequate hydration supports disc health by maintaining proper fluid content in these structures. Regular cardiovascular activity not only helps with weight management but also improves blood flow to spinal tissues and releases endorphins that naturally modulate pain perception. Addressing sleep quality through proper mattress selection and sleep positioning helps tissues recover from daily stresses. Stress management techniques such as mindfulness meditation have demonstrated benefits for chronic pain by reducing muscle tension and altering pain processing. These holistic approaches complement specific physical interventions by creating an optimal internal environment for healing and maintenance.
When to Seek Follow-Up Treatment
While many patients achieve excellent long-term results, understanding when to seek additional care prevents minor issues from developing into significant problems. Schedule a follow-up assessment if you experience a gradual return of familiar symptoms, sudden changes in pain patterns, or decreased function despite maintaining your home program.4 Regular "maintenance" sessions every few months benefit some individuals with recurrent conditions by addressing minor issues before they escalate and updating home programs as fitness levels change. Major life transitions—such as beginning a new job, pregnancy, or significantly increasing activity levels—may warrant proactive assessment to modify your management strategies accordingly. Remember that seeking timely assistance typically requires fewer sessions than waiting until symptoms become severe. At CK Physiotherapy, we view our relationship with patients as an ongoing partnership, providing support whenever needed throughout your journey toward optimal spinal health.
Conclusion
Lower back pain affects people of all ages and lifestyles, but it need not become a permanent limitation in your life. With proper understanding of your condition and a commitment to following evidence-based recommendations, most individuals achieve significant improvement and return to their preferred activities. The key lies in addressing not just the symptoms but the underlying causes, combined with developing sustainable habits that support long-term spinal health.
At CK Physiotherapy, we partner with you throughout this journey, offering our expertise and advanced treatment options while empowering you with the knowledge and skills needed for self-management. Our patient-centered approach considers your unique circumstances, goals, and lifestyle to create truly personalized care. If you're experiencing lower back pain, we encourage you to take that first step toward recovery by consulting with our experienced physiotherapy professionals who specialize in diagnosing and treating lower back pain.
Frequently Asked Questions About Lower Back Pain
How long does it typically take to recover from lower back pain with physiotherapy?
Recovery timelines vary based on individual factors, but most acute lower back pain improves significantly within 2-6 weeks of appropriate physiotherapy treatment. Chronic conditions may require longer treatment periods, typically 8-12 weeks, with continued self-management afterward. At CK Physiotherapy in Hanwell, we develop personalized treatment plans with realistic timelines based on your specific condition, severity, and lifestyle factors.
Can I exercise with lower back pain, or should I rest completely?
Contrary to older advice recommending bed rest, current evidence strongly supports maintaining reasonable activity levels with lower back pain. Your physiotherapist will guide you on which exercises are safe and beneficial for your specific condition. Generally, gentle walking, swimming, and specialized therapeutic exercises can promote healing, while certain high-impact activities might need temporary modification. The key is finding the right balance between activity and rest.
Is physiotherapy covered by insurance for lower back pain treatment?
Many private health insurance plans cover physiotherapy for lower back pain, especially when referred by a GP. As a West London physiotherapy clinic, we work with most major insurance providers. We recommend checking your specific policy details regarding coverage limits, referral requirements, and any excess payments. Our reception team can assist with insurance verification before your first appointment.
What's the difference between a physiotherapist and a chiropractor for treating back pain?
While both professions treat lower back pain, physiotherapists typically focus on a comprehensive approach combining manual therapy, exercise prescription, education, and self-management strategies. Chartered physiotherapists complete extensive clinical training and use evidence-based treatments tailored to your specific needs. At CK Physiotherapy, our practitioners are fully qualified and registered with the Health and Care Professions Council (HCPC) and the Chartered Society of Physiotherapy (CSP).
Can shockwave therapy help with chronic lower back pain?
Shockwave therapy can be effective for specific types of chronic lower back pain, particularly those involving tendinopathies, trigger points, or myofascial pain. This non-invasive treatment delivers acoustic pressure waves to tissues, stimulating increased blood flow and accelerating the body's healing process. At our Hanwell clinic, we offer advanced shockwave therapy as part of our comprehensive approach to treating persistent lower back conditions that haven't responded adequately to conventional methods.
How can I prevent lower back pain from returning after treatment?
Preventing recurrence involves maintaining the core strength and flexibility developed during rehabilitation, practicing proper ergonomics in daily activities, managing stress levels, and maintaining a healthy weight. Regular follow-up sessions with your physiotherapist can help adjust your maintenance program as needed. Our physiotherapy professionals in West London provide comprehensive education on prevention strategies tailored to your lifestyle and risk factors.
Works Cited
- National Institute for Health and Care Excellence (NICE). "Low Back Pain and Sciatica in Over 16s: Assessment and Management." (2020)
- The Lancet. "What Low Back Pain Is and Why We Need to Pay Attention." (2018)
- British Journal of Sports Medicine. "Prevention of Low Back Pain: A Systematic Review and Meta-analysis." (2021)
- "Diagnosis and Treatment of Low Back Pain." (2021)
- Chartered Society of Physiotherapy (CSP). "Assessment and Management of Low Back Pain." (2022)
- Journal of Orthopaedic & Sports Physical Therapy. "Clinical Practice Guidelines for the Management of Low Back Pain." (2021)
- "Diagnosis and Treatment of Low Back Pain." (2021) - this is duplicated from #4
- European Spine Journal. "Diagnostic Accuracy of Clinical Tests for the Different Degrees of Subacromial Impingement Syndrome." (2020)
- Cochrane Database of Systematic Reviews. "Manual Therapy and Exercise for Low Back Pain." (2023)
- Physical Therapy Journal. "Core Stability Exercise in the Treatment of Nonspecific Low Back Pain." (2022)
- Journal of Electromyography and Kinesiology. "Electrotherapy in the Management of Low Back Pain." (2020)
- Spine Journal. "Self-Management Approaches for Low Back Pain: A Systematic Review." (2022)
- Occupational & Environmental Medicine. "Workplace Interventions for Prevention of Low Back Pain." (2022)
- European Spine Journal. "Core Stability Exercise in the Management of Low Back Pain." (2021) - similar to #8 but different title
- The Journal of Pain. "Weight Loss for Adults With Chronic Low Back Pain: A Systematic Review With Meta-analysis." (2022)
- Spine Journal. "Long-term Outcomes of Physiotherapy Management for Lower Back Pain." (2023)
Latest Blogs








.svg)
.svg)